SEX, PLEASURE & MENOPAUSE:
WHAT’S THE ROLE OF TESTOSTERONE?

In this page, I provide some further information on menopause and sexual pleasure. Including:
The changes which happen through perimenopause and menopause
The role of hormones in sexual difficulties around the time of menopause
The treatments available which can help including:
Vaginal moisturisers and lubricants
Vulvo-vaginal (localised) Oestrogen
Systemic HRT (also known as Menopausal Hormone Therapy)
Testosteorne
Changes with menopause
As women go through perimenopause (the years in the lead up to a woman’s final period), hormone levels are very variable. By the time of menopause, the amount of oestrogen in the body has reduced significantly. Testosterone decreases by about 25% between the ages of 30 and 50.
The reduced oestrogen and testosterone leads to decrease blood flow to the vagina, vulva and breasts. The vaginal lining (mucosa) becomes significantly thinner. The clitoris shrinks and becomes less sensitive. As well as affecting the vulva and vagina, oestrogen is also important for bladder health. As oestrogen levels fall, the bladder thins with weakening of the muscles which control the bladder.
These changes can lead to symptoms including:
- vulval itching
- vaginal dryness and reduced lubrication
- reduced sensation & sensitivity from sex
- pain during sex
- reduced sexual desire
- urinary problems such as needing to go to the toilet frequently, urinary incontinence and frequent urinary infections
All the above changes can mean sex can often be less pleasurable. Pain, vaginal dryness, and worries about urinary incontinence during sex can all lead to less pleasure and less desire for sex as a result. There is often a strong hormonal component to symptoms which when treated leads to a relief of symptoms.
However, hormones at not the only factor. Menopause is often a time of change and re-evaluation for some women. Other issues which can play a part include:
- relationship difficulties & differences in sexual desire within couples
- how we feel about our bodies as we age
- anxiety about sex and sexual arousal
- sex not being very rewarding, having sex which doesn’t meet our sexual needs
- cultural and social norms about what is ‘normal’
- our understanding of how desire and sex drive should be
- illness including cancer and medical treatment
- childbirth & fertility issues
- wider mental health issues such as anxiety and stress
- medication, including antidepressants, hormonal contraceptives, medications for bladder issues
These are just some examples. It’s important to put things into this wider context when thinking about medication as oestrogen and testosterone won’t address many of these wider factors.
Sexual difficulties - what role do hormones play?
Treatment - what helps?
It can seem like it’s all very difficult and overwhelming but there is hope. There are lots of things which can help, getting you back to feeling yourself again as well as improve your experience of sex.
Firstly, just by noticing and asking questions such as “what’s happened to my sex drive?!” you can become more aware of what is going on in your body, mind, relationship, and sex life and find a way forward. Usually an approach which addresses different aspects of your current experience at once is the most helpful. Exploring with a psychosexual therapist, or through books, apps and websites as well as ensuring biological aspects are treated is often helpful.
Vaginal moisturisers and lubricants
Vaginal moisturisers can really help symptoms of vulvo-vaginal dryness.
Experiment with a few different products to find one which works for you.
A good quality lubricant for play is also important. Throw the KY jelly in the bin and invest in something more suitable. Here are a few trusted brands.
Topical oestrogen
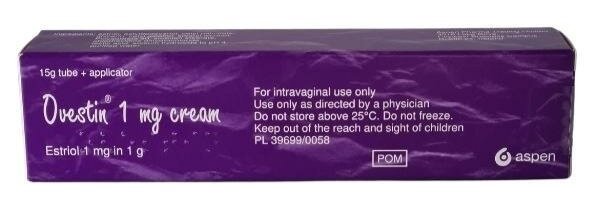
Topical oestrogen delivered locally to the vagina and vulva is helpful in reducing symptoms of itching, burning, pain during sex and urinary symptoms.
Topical oestrogen is incredibly safe as the dose is so low and so little is absorbed into the rest of the body. One year’s worth of oestrogen to the vagina, is the same as one single tablet of HRT taken by mouth.
Sometimes local oestrogen is needed in combination with a systemic (tablet or skin based) HRT.
Vagirux is great as it only has one piece of plastic as an applicator which is reusable and so is more environmentally friendly than only brands such as Vagifem.
Systemic HRT
Oestrogen and progesterone are the basic components of HRT or Menopausal Hormone Treatment (MHT). Sometimes local oestrogen to the vulva and vagina is not enough to help improve symptoms. It also doesn’t help symptoms such as brain fog and hot flushes. This is where systemic HRT comes in.
We know that oestrogen given through the skin (using a gel or patch) is safer than oestrogen given by mouth. Oestrogen given through the skin also has less of a negative effect on testosterone levels.
The type of progesterone given also makes a difference both to the risk of clots in the legs or lungs and breast cancer risk. Different progesterones can also affect testosterone levels. A body identical progesterone such as utrogestan or a mirena coil are the safest types of progesterone and have the least impact on testosterone levels.
Testosterone
Current guidelines recommend that hormone replacement therapy with oestrogen (in combination with progesterone if needed) should be used first before considering testosterone.
Some people don’t absorb hormones through the skin as well as others, and so it is always worth doing a blood test to check oestrogen levels on HRT and your natural testosterone level before considering adding testosterone replacement. For some women, adequate oestrogen replacement stops vulval & vaginal irritation which stops sex being painful. This then leads to an increase in sexual pleasure and desire.
However, if despite adequate oestrogen and if there are no obvious other psychological, social or relationship factors causing low desire, it is reasonable to have a trial of testosterone therapy to see if this helps symptoms. This is usually a testosterone gel applied to the skin each day, equivalent to an eighth of the dose for men. There are very few risks to testosterone therapy as long as it is under the supervision of an experienced doctor, with monitoring of blood testosterone levels after three weeks or so, to check levels don’t become too high.